Ophthalmologist | 8 min read
Keratoconus: Symptoms, Complications and Treatment
Medically reviewed by
Table of Content
Synopsis
Keratoconus is a degenerative eye illness which can be caused due to genetic factors and age. This blog talks about the severe eye disease Keratoconus and everything from its causes and symptoms to its treatment in detail.
Key Takeaways
- Keratoconus is an eye disease caused by abnormalities in the cornea
- Family history and age is a significant reason for this issue
- There are three stages involved in the treatment of Keratoconus
Keratoconus is a condition best described by the thinning of the cornea and abnormalities of the cornea's surface. The cornea is the front of your eye's transparent outer layer. The cornea's middle layer, which is also its thickest layer, is mainly composed of water and the protein collagen. The collagen helps maintain its standard, rounded shape and keeps it robust and flexible. A cornea that is in good health allows you to see well. However, the cornea thins and bulges into an atypical cone form in Keratoconus, impairing vision.
In most cases, Keratoconus starts after adolescence and develops until the mid-30s. It is impossible to predict whether or how rapidly the disease will advance. Both eyes are frequently impacted by Keratoconus, though one is usually more severely impacted than the other. It may affect vision in the following ways:
- The cornea's changing shape brings progressive near-sightedness and irregular astigmatism, leading to impaired vision
- Glare and light sensitivity are also frequent side effects
- Every time a keratoconus patient visits their eye doctor, their prescription for glasses frequently changes
What Causes Keratoconus?
The specificities of keratoconus causes remain unknown. According to researchers, certain people are more likely to be born with it. It is a complicated eye disorder called Keratoconus and is probably brought on by hereditary and environmental factors.[1] Several factors given below might be able to answer what causes this issue:
Family history
Your risk of developing this ailment is higher if someone in your family already has it. Starting at about age 10, get your children's eyes tested for symptoms if you have it. A family history of glaucoma can also result in Keratoconus. Being a significant eye-related issue, World Glaucoma Week is observed to spread awareness about it.
Age
It commonly begins in your teenage years. However, it may not manifest till you are 30 years old, or it may do so sooner. People over 40 can also be affected, but this is less typical. Studies[2] have revealed a link between systemic illnesses such as retinitis pigmentosa, Ehlers-Danlos syndrome, osteogenesis imperfecta, Down syndrome, and Keratoconus.

Inflammation
The cornea's tissue can be destroyed by inflammation brought on by conditions such as allergies, asthma, or atopic ophthalmia.
Rubbing your eyes
Excessive rubbing of the eyes over time might damage the cornea. In addition, if you already have Keratoconus, it may potentially hasten its progression.
Race
Research including over 16,000 keratoconus patients indicated that Black or Latino patients are 50% more likely to get the condition.[3]
Symptoms of Keratoconus
Although both eyes are frequently affected by Keratoconus, one eye may be worse than the other (asymmetric). Symptoms can include, but do not always include:
- Slight eyesight distortion and blurriness
- Double vision or light streaks (or "ghost" pictures)
- Increased sensitivity to glare and bright light
- Issues with driving at night
- Eye irritation, eye pain-related headaches, or eye-related redness
Typically, the keratoconus symptoms start in late adolescence and last for 10–20 years. However, due to the disease's progressive nature, the cornea may gradually swell and create issues with eyesight. For this reason, you might need to replace your prescription glasses regularly. In addition, small corneal fissures that result from bulging can occasionally produce edema and the appearance of a white eye (hydrops). An individual may feel a sharp decline in eyesight if this happens.
Additional symptoms of advanced-stage Keratoconus include:
- Blurry or distorted vision as well as steadily declining near-sightedness (the ability to see things clearly in the distance) (irregular astigmatism)
- It cannot use duplicate contacts because they might not fit correctly. In addition, corneal hydrops may cause severe discomfort. Therefore, corneal transplantation should be carried out immediately if this problem is present
- If you notice any of these symptoms, make an appointment with a doctor of ophthalmology to have your eyes examined. It's also important to remember that eye diseases can develop before symptoms, making frequent and timely eye exams even more crucial
How is Keratoconus Diagnosed?
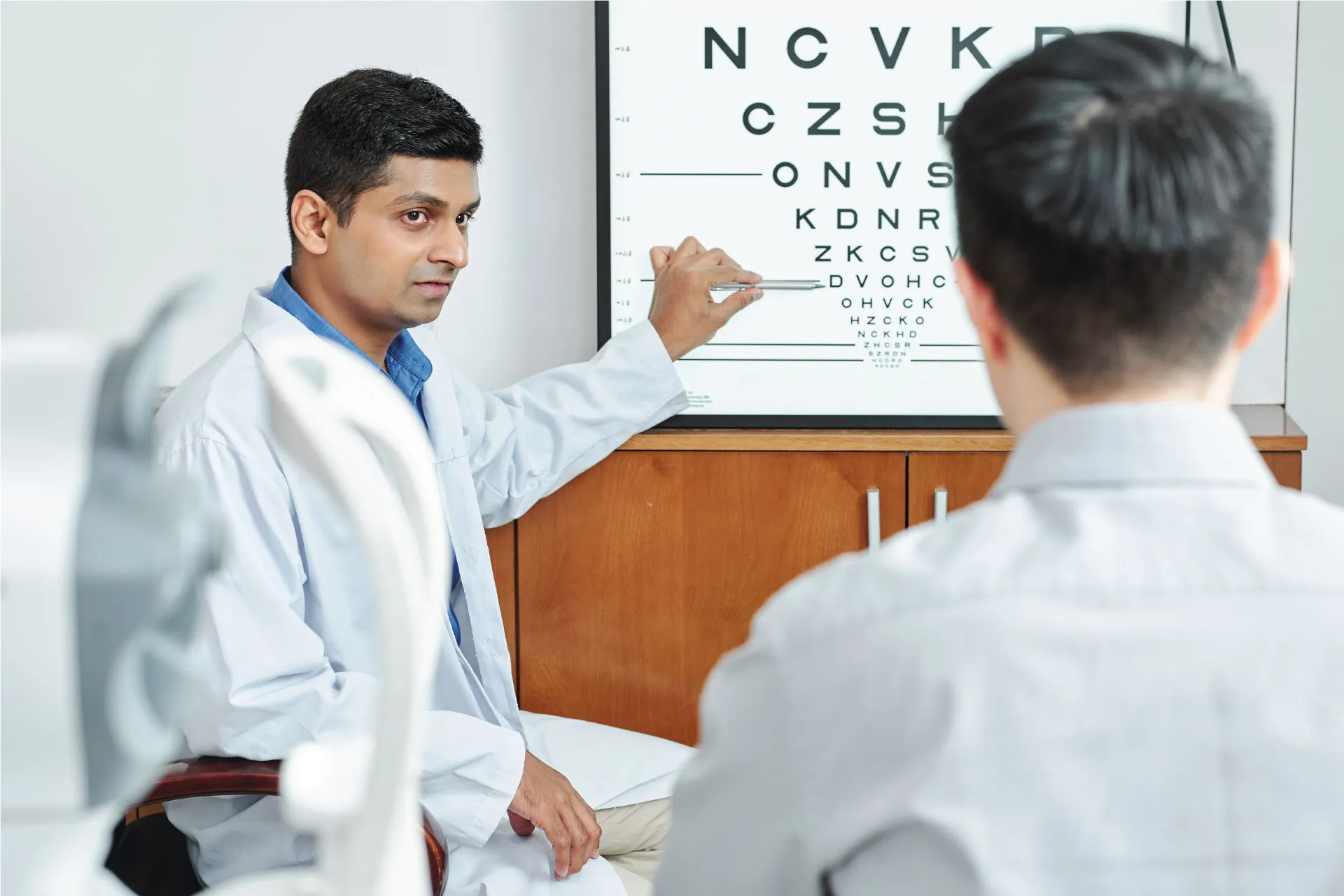
If you are wondering how it is diagnosed, then, in that case, Keratoconus can be diagnosed with the help of a routine eye exam. A conversation with your eye doctor about your primary vision issues and a discussion of your medical and family histories can also help. Your doctor must evaluate the corneal curvature and perform an astigmatism test to rule out irregular astigmatism.
From the age of 10, children with one or both keratoconus-affected parents should get annual eye exams to determine whether the condition is developing in them as well. The following tests may be used to identify Keratoconus by your doctor or optometrist:
- With a microscope and a light beam focused on the eye's surface, a slit-lamp examination looks for abnormalities in the cornea's size or shape
- With keratometry, you can see if your cornea is irregularly shaped by focusing a laser beam on it and measuring the reflection. They could also use an ophthalmometer or a hand-held keratoscope, which are additional instruments that can thoroughly examine the cornea
- Pachymetry is the measurement of corneal thickness. Computerized corneal mapping involves projecting light rings onto the cornea's surface, which the cornea then reflects and reveals information about the surface's shape and structure
Some Keratoconus Related Disorders
Several diseases and conditions can resemble Keratoconus, including:
- Pellucid marginal degeneration (thinning and steepening of the cornea's outer edges)
- Keratoglobus (thinning of the cornea with a globe-shaped or spherical appearance)
- Interstitial Keratitis (chronic damage to the cornea's deep layers)
- Corneal dystrophies (a group of inherited, frequently progressive eye diseases that allow for the accumulation of foreign materials inside the cornea)
Keratoconus Treatment
The course of keratoconus treatment depends on the disease's stage and focuses on eyesight correction.
Initial Stages
In the early phases of keratoconus therapy, glasses are used to correct astigmatism and near-sightedness. However, glasses cannot provide patients with clear vision as Keratoconus develops and advances, necessitating a contact lens, often a hard contact lens.
Developing Stages
Cross-linking the corneal collagen is a treatment option for progressive Keratoconus. A vitamin B solution is applied to the eye during this one-time treatment, after which the eye is exposed to UV radiation for no more than 30 minutes. New collagen linkages are formed due to the solution, restoring and maintaining some of the cornea's strength and shape.
The procedure can prevent eyesight from worsening and, in certain situations, may even enhance vision, but it cannot completely restore the cornea's natural function. For efficient riboflavin permeation of the corneal tissue, the treatment may need the removal of the cornea's thin outer layer (epithelium).
Higher Stages
- Corneal Ring: A regular contact lens may become too unpleasant to use if you have severe Keratoconus. Intacs are plastic, implanted C-shaped rings that flatten the cornea's surface to enable better vision. They could also provide a better fit for contact lenses. About 15 minutes are needed for the operation
- Cornea Transplant: A donor cornea replaces the patient's injured cornea during a corneal transplant. Following the transplant, vision is often hazy for three to six months, and medication is required to prevent transplant rejection. For the best eyesight after transplant surgery, glasses or contact lenses are nearly always necessary
Can Keratoconus Damage Vision?
Your eye may become unable to focus without the aid of glasses or contact lenses if the cornea changes. You could require a corneal transplant to regain your vision if the problem worsens. If you have Keratoconus, laser vision correction surgery, or LASIK, is risky. Your cornea may become more fragile, and your eyesight may get poorer. Do not have a LASIK surgery even if you only have a slight degree of Keratoconus.
Additional Read: Complete Health Solution Plans
Complications Of Keratoconus
In rare circumstances, your cornea may suddenly enlarge, resulting in an abrupt reduction in vision and corneal scarring. This is brought on by a disorder that causes the cornea's internal lining to tear, enabling fluid to enter the cornea (hydrops). The swelling often goes down on its own, but a scar that impairs your eyesight may develop. In addition, your cornea may develop faults due to advanced Keratoconus, especially in the areas where the cone is most noticeable. A corneal scar exacerbates visual issues and may necessitate corneal transplant surgery.
How to Recover from Keratoconus?
You may be able to use contact lenses to maintain your visual function with early diagnosis and rapid corneal cross-linking treatment. With a corneal transplant, your chances of recovering quickly and leading an everyday, active life are pretty good. Contact lenses will be a part of your vision rehabilitation, and you could require long-term steroid maintenance therapy. It has been observed that Keratoconus can progress and return after receiving a corneal transplant. However, it is unclear how frequently this might happen. You can also resort to Yoga for eyes and other exercises that help with your vision and minimize the effects of this ailment.
Additional Read: Amazing Benefits of AnjaneyasanaIf your eyesight rapidly deteriorates, it may be due to an abnormal eye curvature. Consult an ophthalmologist or optometrist (astigmatism). During routine eye exams, they might also search for keratoconus symptoms.
For more information and help, contact Bajaj Finserv Health to speak to an ophthalmologist and get a doctor consultation. In addition, you can schedule consultations from the comfort of your home to receive the right advice regarding keratoconus surgery.
References
- https://pure.ulster.ac.uk/en/publications/association-of-genetic-variation-with-keratoconus
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3353679/
- https://ihpi.umich.edu/news/largest-ever-study-cornea-condition-reveals-hidden-risk-factors-u-m-team-reports
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.