Ent Surgeon | 7 min read
Parosmia: Causes, Symptoms, Diagnosis and Treatment
Medically reviewed by
Table of Content
Synopsis
This health condition, parosmia, requires you to be careful about the situations which put you to lose your sense of smell. Parosmia can be treated if you are careful about the symptoms and precautions. Read this blog for more information about Parosmia.
Key Takeaways
- Parosmia is frequently linked to brain trauma or infection
- Parosmia is brought on by a brain tumor, a sinus polyp, or an early symptom of other neurological diseases
- Long-term prognosis for people with parosmia depends on age, gender, and how good sense of smell
When the olfactory sensory neurons, which are smell receptor cells in your nose, cannot correctly detect and convey smells to your brain, such a condition is known as Parosmia. Your sense of smell can become distorted if you have Parosmia. There are several distinct types of Parosmia that people might encounter. When your brain picks up on strong, unpleasant scents, Parosmia can make you physically ill in the most extreme situations.
Olfactory impairment may prevent a person from being able to experience the variety of smells in their surroundings. Or the aromas they pick up the scent "off." For instance, warm cookies from the oven may smell sweet and delectable to most people but rotten and unpleasant to those with Parosmia. When you sniff a banana, your nose detects rotting flesh rather than a delicious, pleasant scent. Infection with a virus frequently results in Parosmia.
Additional Read: Neurocognitive Disorders
For some people, parosmia meaning is synonymous with anosmia. Anosmia, however, describes a complete loss of scent perception. Common COVID-19 symptoms are anosmia and Parosmia, including dysgeusia (a distorted sense of taste) and ageusia (a total loss of sense of taste) [1].
Olfactory dysfunctions are divided into two groups: qualitative (e.g., parosmia and phantosmia) diseases that describe a subjective change in smell quality and quantitative (e.g., anosmia and hyposmia) illnesses that quantify an objective variation in the ability to smell. For example, a total lack of smell is referred to as anosmia, while a diminished sense of smell is hyposmia. In contrast, phantosmia happens when someone thinks they can smell something that isn't there.
The olfactory bulb, located in the nasal cavity on the anterior aspect of the frontal lobe, is generally responsible for the sense of smell (i.e., the brain lobe that controls behavior and emotion). In the cerebral hemispheres, the primary olfactory cortex receives information from olfactory bulb neurons (i.e., the outermost portion of the brain). Therefore, Parosmia may result from harm to the olfactory bulb or interruption along this neuronal pathway.
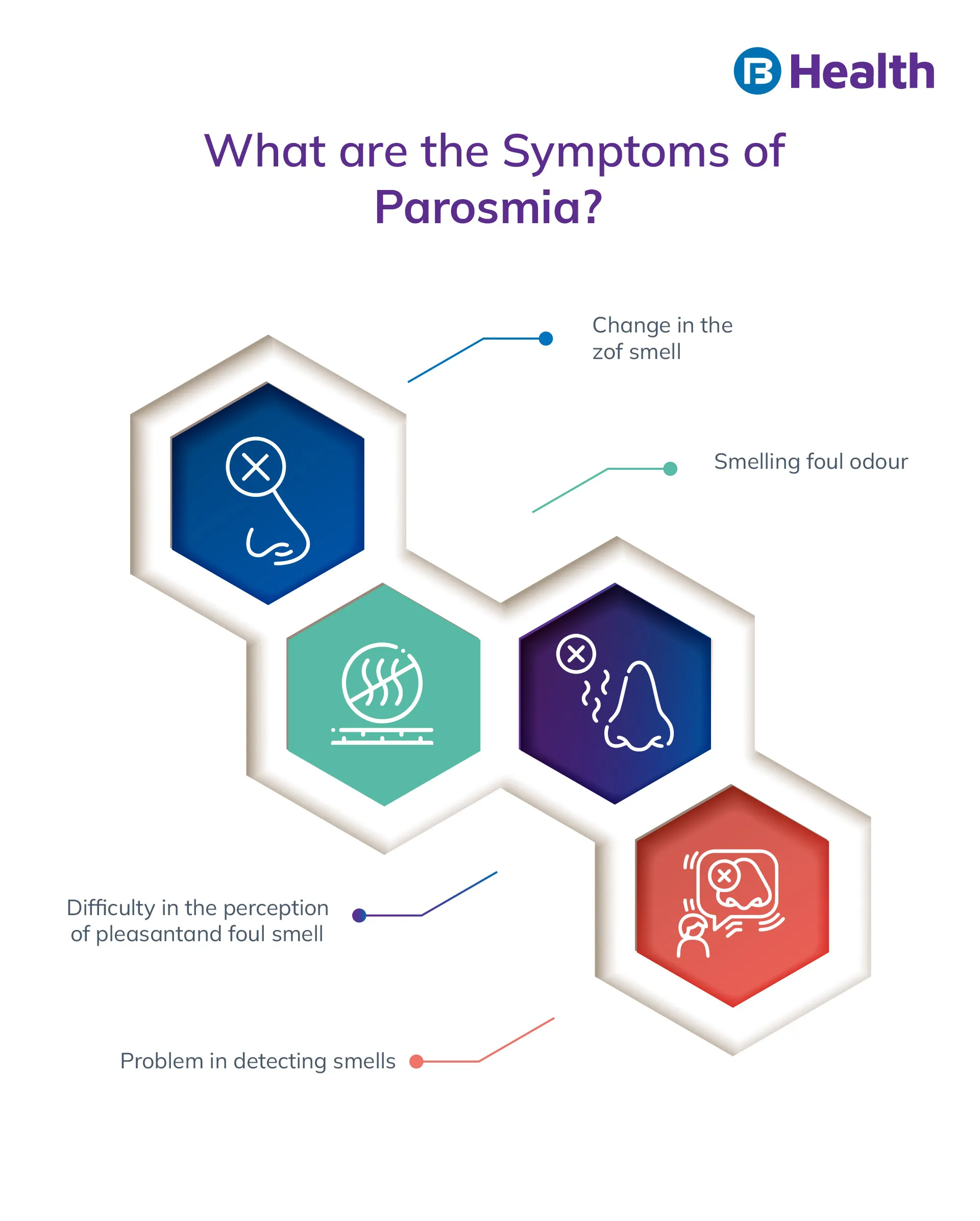
Symptoms of Dysosmia
The symptoms of Parosmia result in Olfactory dysfunction. Different people experience different parosmia symptoms. Some illnesses are minor and transient. Others are harsh and protracted. Most of the time, dysosmia symptoms appear after an infection has healed. Anosmia, the total loss of smell, is not the same as Parosmia. Those who have Parosmia could:
- They have difficulty identifying specific smells in their environment due to olfactory neuron damage.
- A foul smell, especially when food is present.
- Previously pleasant smells may now be overbearing and unpleasant.
- You can lose your appetite due to the disease because food doesn't taste as delicious as it used to.
- This could imply that items you once liked may no longer be edible because of strong, unpleasant scents that can make you nauseous.
- Sometimes people can have ear infection symptoms and strep throat symptoms because of bacterial infections.
Causes of Olfactory Impairment
Parosmia typically happens after a virus, or another medical condition damages your odor-detecting neurons, generally known as your olfactory senses. Your brain receives instructions from these neurons that line your nose on how to interpret the chemical data that makes up smells. As a result, the way odors enter your brain is altered when these neurons are damaged.
These neurons provide signals to the olfactory bulbs underneath the front of your brain, which informs your brain about the scent and whether it is pleasant, seductive, tasty, or offensive. Dysosmia can result from injury to these olfactory bulbs. Parosmia can cause by several various conditions, such as:
- COVID-19 infection
- Severe sinusitis
- Head trauma
- Brain injury
- Polyps in the nose
- Viral or bacterial infection
- Neurological disorders
- Upper respiratory illnesses, such as colds
- Influenza (flu)
- Specific medicines
- Constant mouth drying (xerostomia)
- Smoking
- Chemical exposure
- Cancer Therapies
- Seizures in the temporal lobe
- Exposure to toxins
- Brain tumors (less common)
Diagnosis and Tests for Parosmia
The diagnosis of Parosmia cannot be made with a specific test. To rule out additional reasons for smell dysfunction, such as anosmia or hyposmia, where your ability to smell things is diminished or impaired, your doctor will typically interview you about your symptoms and perform some tests. An otolaryngologist can diagnose Dysosmia, commonly known as an ENT surgeon or ear, nose, and throat physician.
Additional Read: Ear Infections
Your doctor can show you different items and ask you to rate their quality and describe their scent. A little booklet of "scratch and sniff" beads that you respond to while being observed by a doctor is a typical test for Parosmia. Your physician might inquire about the following during the visit:
- the prevalence of cancer and neurological disorders in your family
- any infections you may have recently had
- Personal habits, like smoking
- Medications you take at the moment
Your doctor might advise more testing if they think a neurological condition or cancer may be the root of your olfactory impairment. This might involve:
- a sinus CT
- a sinus biopsy
- an MRI
Treatments for Parosmia
Dysosmia can sometimes be cured, but not always. Your sense of smell may return to normal if environmental conditions, medications, cancer treatments, or smoking are the root causes of your Parosmia.
The following are some parosmia treatments:
- A vitamin
- antibiotics
- Zinc
Your doctor might occasionally recommend medication to treat the symptoms of Parosmia. Although further research is needed, studies have shown that these medications could help you regain your sense of smell:
- Phenytoin.
- Clonazepam.
- Topiramate.
- Valproic Acid
Additional research and case studies are required to prove that these are more beneficial than a placebo. Consider olfactory training therapy if your olfactory impairment persists and affects your appetite and weight. This sort of therapy, also called "smell training," is purposefully inhaling four distinct odors for up to 15 seconds. For several months, the procedure is carried out twice every day.
To treat Parosmia, surgery may sometimes be required. The damaged sensory receptors in your nose, such as polyps or tumors, can be removed by a surgeon to restore your ability to smell. But because this parosmia treatment is so complicated, the hazards frequently outweigh the benefits. To determine the best treatment options, you must speak with your doctor.
Is it possible to prevent Dysosmia?
It is impossible to prevent Parosmia because it frequently results from trauma, viruses, and other uncontrollable circumstances. However, if environmental triggers like smoking or chemical exposure cause Parosmia, eliminating those variables should lessen or immediately prevent your symptoms. Wash your hands often and adhere to all U.S. Centres for Disease Control and Prevention (CDC) recommendations and guidelines to lower your risk of bacterial and viral-related Parosmia.
How long does Parosmia last?
Those who have Parosmia typically suffer symptoms for a while longer than two weeks. The specific cause of Dysosmia in COVID-19 is unknown. Most patients with this symptom are thought to have also lost their sense of taste and smell when they were ill. Its duration is also a mystery. According to research, a parosmia episode typically lasts three months, while some cases can last up to six months. However, the underlying etiology significantly impacts how long the symptoms last.
Parosmia is a disorder that causes your olfactory perception to be warped. As a result, odors previously seen as pleasant will suddenly smell unpleasant or rotting. Dysosmia can result from various illnesses, including infections, chemotherapy, radiation treatment, chemical exposure, neurological disorders, and COVID-19 recovery. It cannot be treated universally and frequently goes away after the underlying cause is managed. Parosmia may have long-term repercussions, such as altered scent, weight loss, and starvation. If you are experiencing parosmia symptoms, seek assistance from a physician or other medical expert.
You can get doctor consultations online with a click on Bajaj Finserv Health. They have doctors for hearing loss treatment which can be caused by the effects of Parosmia or olfactory impairment. The best thing here is that you can book a teleconsultation from the comfort of your home and get all the advice you need online. With the convenience and safety this offers, you can start taking the best care of your health and diet. If you want to protect yourself from any disease, you can avail of health insurance policy.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8618742/#:~:text=In%20conclusion%2C%20COVID%2D19%2D,losses%20of%20smell%20and%20taste.
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.