Covid | 9 min read
Black Fungal: Symptoms, Causes, Treatment, Prevention
Medically reviewed by
Table of Content
Key Takeaways
- Mucormycosis is an invasive fungus caused by a group of moulds called mucormycetes
- This fungus is usually found in the soil, decaying fruits, vegetables, plants, and manure
- Early diagnosis and treatment is the key to a complete cure without severe complications
After detecting the first coronavirus case in January last year, India went into a strict 55-day nationwide lockdown. Despite it, by June India was the third-worst affected country in the world. While the number of cases in the country dropped over time, with fewer restrictions and overall complacency, the second wave of the novel coronavirus halted the country’s momentum towards normalcy.
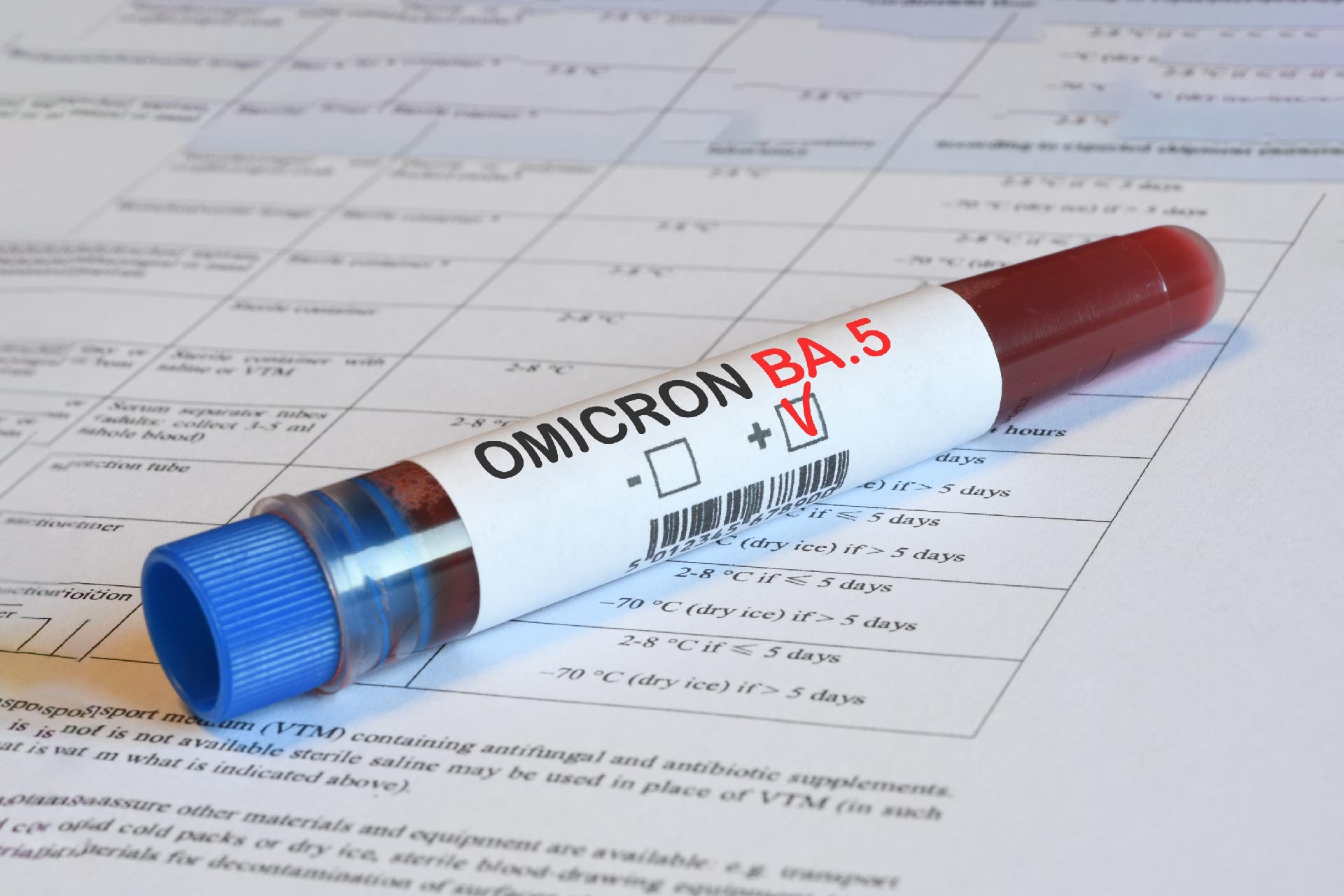
Furthermore, the acute shortage of vaccines has resulted in a slower vaccination drive in most states. The second wave also saw the rise of Covid-19 cases in the younger population, including children. The presence of the new B.1.617 variant of the virus has further aggravated the situation. This variant further mutates into E484Q and L452R and can evade antibodies in the immune system and become resistant to the virus. The variant has been found in more than 60% of samples in Maharashtra, one of the worst-hit states in the country.
As our healthcare system tries to deal with the increasing caseload of Covid-19 cases, doctors across states are reporting an increasing number of black fungus or mucormycosis cases in those recovering from Covid-19. With the alarming rise in black fungal infection in India, the Indian Council of Medical Research (ICMR) has notified doctors across the country to look for black fungal infection symptoms in Covid-19 patients. This aggressive and fatal infection usually affects people with a weakened or compromised immune system, a common occurrence in patients that recover from the coronavirus, making them highly susceptible.
It is important to understand the spread of black fungus in India, especially if you have diabetes, kidney disorders, or cancer. Read on to know more about black fungal disease causes, symptoms, treatment, and prevention.
Also Read: How to Boost your Immune SystemWhat is Black Fungal?
Mucormycosis is an invasive fungus caused by a group of molds called mucoromycetes. This fungus is usually found in the soil, decaying fruits, and vegetables, plants, and manure. It is also found in the air and the mucus of healthy people. Generally, inhaling these spores can cause fungal infection, attacking your sinuses and lungs.
Mucormycosis is an opportunistic infection that infects and thrives in people with a compromised or weakened immune system. In such people, the infection spreads rapidly, having a crippling impact on their health. While it has a mortality rate of only 50%, there is a rise in cases of black fungus in Covid patients because Covid-19 severely depletes the immune system. Therefore, states and cities worst hit by Covid-19 are hotspots for black fungal disease in India. For example, Mumbai in Maharashtra has reported more than 2000 cases and eight deaths due to this Covid fungal infection. Furthermore, those with diabetes, undiagnosed high blood pressure, kidney conditions, and other comorbidities that weaken the immune system further while being diagnosed with Covid-19 are at an increased risk of contracting this black fungal infection.
Also Read: How to keep your kids safe from Coronavirus
Connection Between Covid-19 and Mucormycosis
Typically, the fungus can enter the body either through a cut or bruise or through the nose. On entering the body through a cut or any skin trauma, it causes local infection in the body. However, if the fungus enters the body through the nose, it can travel to the lungs, affecting the sinuses, eyes, and eventually the brain, proving fatal. However, so far, there are multiple beliefs regarding the rise of cases of black fungus in India. Some doctors believe this is due to the rampant use of steroids, one of the life-saving treatment options for critically ill Covid-19 patients.
Steroids are administered to reduce inflammation in the lungs caused by the coronavirus. However, while it prevents and stops the damage caused by the virus, it weakens the immune system in diabetic and non-diabetic patients. This weakened immune system is believed to be the trigger for mucormycosis.
Other causes include administering medication to at-home Covid patients without checking their blood sugar levels since black fungus thrives on sugar. Patients returning to unhygienic living conditions after recovering from Covid are also at risk. The use of tap water and tainted oxygen pipes while delivering oxygen therapy are also cited as the cause of black fungus infection in India.
Who Is at Risk?
While the condition can affect anyone, certain groups of people are more at risk than others.
Those with weakened immune systems are more susceptible to black fungal infection. This includes people with HIV/AIDS, cancer, or taking certain medications that suppress the immune system.
People with diabetes or other chronic medical conditions that cause poor circulation are also at increased risk. This is because the fungus that causes the black fungal infection thrives in warm, moist environments.
If you have any of these risk factors, it’s important to be extra vigilant about hygiene and to seek medical help if you develop any symptoms of black fungal infection.
Black Fungus Symptoms
Early diagnosis and treatment is the key to complete cure without severe complications. So, if you see any of the following black fungal disease symptoms, rush to the doctor immediately.
- Nasal congestion or blockage
- Blackish or bloody nasal discharge
- A localized pain in the cheekbone
- Experiencing pain, numbness, and swelling
- Experiencing pain only on one side of the face
- Presence of blackish decolorization on the bridge of the nose or palate
- Thrombosis and development of necrotic skin lesions
- Loosening of teeth and experiencing trouble with jaw movement
- Experiencing sudden double or blurred vision
Other symptoms include the onset of chest pain, aggravation of respiratory symptoms, and pleural effusion.
Also Read: How to deal with CoronavirusBlack Fungus Causes
Mucormycosis is a rare but potentially fatal fungal infection. It most commonly affects people with weakened immune systems, such as those with cancer or HIV/AIDS. It can also occur in people who have recently had surgery, been on long-term steroids, or are diabetic.
The fungus that causes mucormycosis, Mucorales, is found in soil, air, and water. It can enter the body through the nose, mouth, or skin. Once inside the body, the fungus can spread to the brain, lungs, and other organs.
Mucormycosis is often mistaken for a cold or sinus infection. Early symptoms include headaches, fever, and congestion. As the infection progresses, it can cause blackening and death of tissue (necrosis), especially in the sinuses, lungs, and brain.
Treatment for mucormycosis is typical with antifungal medication. Surgery may also be necessary to remove infected tissue. People with mucormycosis often require hospitalization and intensive care.
How is Black Fungus Diagnosed?
Mucormycosis is a severe fungal infection that can cause serious health complications. Early diagnosis and treatment are important to improve the chances of a good outcome.
There are several ways that mucormycosis can be diagnosed. A doctor may suspect the infection based on the symptoms a person is experiencing. A physical exam can also help to rule out other conditions.
Imaging tests, such as X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI) scans, can be helpful in diagnosing mucormycosis. These tests can show changes in the tissue that are characteristic of the infection.
A biopsy can also help diagnose mucormycosis. This involves taking a small tissue sample from the affected area and examining it under a microscope. This can help to confirm the presence of the fungus.
Blood tests may also be used to help diagnose mucormycosis. These tests can look for changes in the blood that may be indicative of the infection.
If you are experiencing any symptoms indicative of mucormycosis, it is important to see a doctor immediately. Early diagnosis and treatment are important to improve the chances of a good outcome.
Black Fungus Complications
- Mucormycosis symptoms can cause blindness in those afflicted by it.
- Blocked blood vessels or clots
- Nerve damage can make everyday tasks like grasping a cup or a spoon difficult. Some people may have to use a particular utensil to help them grip their food.
Mucormycosis is rare and often deadly. Researchers haven't been able to find the mortality rates with 100% certainty, but they estimate that 54% of people die from the infection. The likelihood of death depends on the part of the affected body. For example, fewer people die from a sinus infection than they do from a lung or brain infection.
Black Fungus Prevention
Mucormycosis is a serious fungal infection that can be deadly if left untreated. Early diagnosis and treatment are critical for the best possible outcome. In order to prevent mucormycosis, it is important to be aware of the risk factors and take steps to reduce your exposure.
Risk factors for mucormycosis include exposure to contaminated soil or water, contact with infected animals, and being immunocompromised. People with diabetes or other chronic medical conditions are also at increased risk. If you have any of these risk factors, it is important to take steps to avoid exposure to the fungus.
Some simple precautions that can help reduce your risk of exposure to the fungus include wearing gloves when gardening or working in contaminated areas, avoiding contact with sick animals, and washing your hands thoroughly after contact with potentially contaminated surfaces. If you have diabetes or another chronic medical condition, it is important to closely monitor your health and seek medical attention at the first sign of any infection.
By taking some simple precautions, you can help reduce your risk of exposure to the fungus that causes mucormycosis. Early diagnosis and treatment are critical for the best possible outcome, so if you think you may have been exposed, don't delay in seeking medical attention.
Treatment for Mucormycosis (Black Fungal Infection)?
Black fungal infection treatment options include multidisciplinary medical expertise ranging from microbiologists, intensive neurologists, and internal medicine specialists to ophthalmologists, ENT specialists, dentists, and surgeons. This is because the infection can spread to the nose, lungs, jaw, and eventually the brain.
The primary treatment option includes surgically removing infected tissues, which in adverse cases may cause a patient to lose their upper jaw or even their eyes. Also, Amphotericin B Liposomal is used to treat black fungus infection. A patient may require 20 vials of this injection and each cost between Rs.5,000 to Rs.6,000. However, there is a severe shortage of this medicine in the market, forcing doctors to conduct surgeries to save lives.
Covid patients with immunosuppressing comorbidities, especially diabetes, are at high risk of contracting mucormycosis. The use of steroids to treat Covid-19 can aggravate diabetes, compromising the immune system, and making the patient susceptible to black fungus infection. Therefore, it is pertinent to ensure that you and your family practice Covid-19 prevention measures of wearing masks, social distancing, washing your hands, and avoiding gatherings. This especially applies to anyone that has pre-existing immunocompromising comorbidities.
To further get expert advice regarding Covid-19 prevention and black fungal symptoms, use the Bajaj Finserv Health. This gives you instant access to specialist doctors close to you, so you can book in-person and e-consultations in seconds. Also get a range of health plans and resources to address your healthcare needs more affordably and in a more informed manner.
References
- https://indianexpress.com/article/explained/mucormycosis-in-covid-patients-fungal-infections-7308721/%22%20/t%20%22_blank
- https://www.sciencedirect.com/science/article/pii/S2211883720301465,
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.