Diabetes | 7 min read
Diabetic Retinopathy: Symptoms, Causes, Types, Treatment
Medically reviewed by
Table of Content
Synopsis
Diabetic retinopathy is a condition caused by diabetes that impacts the eyes. It is caused by damage to the blood vessels in the retina, which is the light-sensitive tissue present at the back of the eye. Although diabetic retinopathy may initially cause no symptoms or minor vision issues, it might eventually result in blindness. Read this article to know more about its treatment and prevention.
Key Takeaways
- Diabetic retinopathy is a condition that affects the retina and impairs eyesight
- Diabetic retinopathy results from a lengthy history of diabetes and inadequate blood sugar level regulation
- Diet and exercise can help control diabetes and keep diabetic retinopathy at bay
What is Diabetic Retinopathy?
In persons with diabetes, a disease known as diabetic retinopathy can result in vision loss and eventual blindness. This is because the retina's blood vessels are impacted (the layer of tissue in the back of your eye, which is light-sensitive).
It's crucial to undergo a thorough dilated eye exam at least once a year if you have diabetes. This eye condition can develop in anyone who has type 1 or type 2 diabetes. [1] The early detection of diabetic retinopathy can help you take action to preserve your eyesight even though it may not initially present with any symptoms.
You may be able to avoid or postpone vision loss by controlling your diabetes with a good diet, regular exercise, and medication. A good lifestyle will also keep other complications of diabetes, like diabetic ketoacidosis, which is life-threatening, away. The most typical cause of vision loss in people with diabetes is also the leading cause of new instances of blindness in adults. [2]
Types of Diabetic Retinopathy
The following are the two types of diabetic retinopathy:
1. Acute diabetic retinopathy
Non-proliferative diabetic retinopathy (NPDR), the more prevalent variant, is marked by the absence of new blood vessel growth.
The retinal blood vessel walls deteriorate when you have NPDR. Small protrusions from the smaller arteries' walls can occasionally leak fluid and blood into the retina. The diameter of larger retinal vessels can also start to enlarge and change. NPDR can worsen when more blood vessels are blocked, from mild to severe.
There may occasionally be an accumulation of fluid (oedema) in the retina's macular region due to retinal blood vessel injury. Treatment is needed to prevent irreversible vision loss if macular oedema impairs vision.
2. Advanced diabetic retinopathy
Diabetic retinopathy, also known as proliferative diabetic retinopathy, can progress to this more severe form. This type results in the development of new, aberrant blood vessels in the retina as injured blood vessels close off. The transparent, jelly-like fluid that fills the centre of your eye can leak from these new blood vessels because they are weak (vitreous).
The retina may eventually separate from the back of your eye due to scar tissue produced by the development of new blood vessels. In addition, the eyeball may become pressurised if the new blood vessels obstruct the normal drainage of fluid from the eye. Glaucoma can develop due to this buildup harming the optic nerve, which delivers images from your eye to your brain.
Additional Read: Sugar-Free Breakfast RecipesCauses of Diabetic Retinopathy
The little blood vessels that maintain the health of your retina are blocked if your blood glucose level (blood sugar) is too high for an extended period of time. New blood vessels will try to form in your eye, but they won't expand properly. The blood vessels begin to deteriorate. Your retina may experience blood and fluid leakage. Macular oedema is a different ailment that may result from this. It may cause hazy vision.
The more blood vessels that are clogged, the worse your disease gets. Because of the additional blood vessels in your eye, scar tissue accumulates. In addition, your retina may tear or separate due to this added pressure. This may also result in blinding eye disorders, including glaucoma or cataracts (clouding of the eye's lens). Blockage of the blood vessels in the body is also how diabetes is related to hypertension.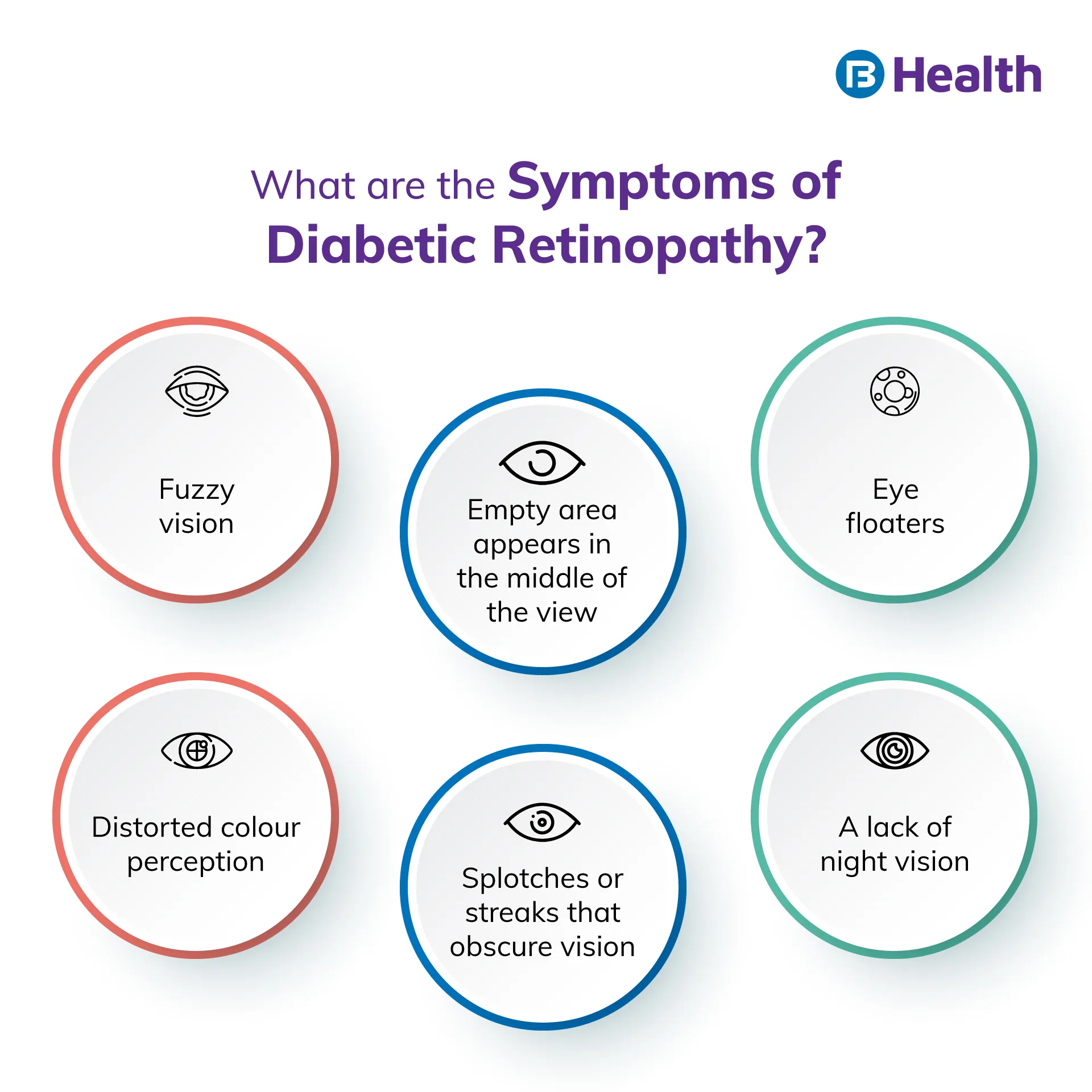
Symptoms of Diabetic Retinopathy
Usually, no symptoms are involved in the initial stages of diabetic retinopathy. However, keeping an eye out for prediabetes is important. But most of the time, when the problem is more severe, symptoms frequently become apparent. Both eyes are commonly affected by diabetic retinopathy. The following are examples of diabetic eye problems that result from this condition:
- Fuzzy vision
- Distorted colour perception
- Eye floaters, also known as translucent spots and black strings, move in the direction that a person is looking and float in their field of vision
- Splotches or streaks that obscure vision
- A lack of night vision
- A shadowy or empty area appears in the middle of the view
- An entire loss of vision occurs suddenly
Additional Read: Eye Floater Causes And Symptoms
How is Diabetic Retinopathy Diagnosed?
Here are some of the methods of diabetic retinopathy diagnosis:
Pupil dilation:
To check for any changes in the blood vessels in your eye or to see if any new ones have grown, your doctor will dilate your pupils. Your retina's swelling and detachment will also be examined.
Fluorescein angiogram:
Your doctor can use this test to determine whether you have severe diabetic retinopathy or DME. It reveals whether any of your blood vessels are damaged or leaking. Your physician will inject you with fluorescent dye into an arm vein. Your doctor can see photographs of the blood vessels in your retina when the dye reaches your eyes and identify any significant issues.
How is Diabetic Retinopathy Treated?
Diabetic retinopathy treatment involves the following:
Anti-VEGF injection therapy
Drugs that inhibit VEGF, a protein that causes abnormal blood vessels to form in your eye, can stop the growth of aberrant blood vessels and reduce fluid buildup in your retina. Aflibercept (Eylea), bevacizumab (Avastin), and ranibizumab are examples of anti-VEGF medications (Lucentis).
Laser surgery for the macular fovea/grid
The vessels in your macula that are leaking are lightly burned by lasers. After this operation, anti-VEGF therapy can be required.
Corticosteroids: These drugs can be implanted or injected into your eye by a doctor. There are both long-acting and short-acting varieties. Steroids can increase your risk of developing cataracts or glaucoma. If you take them, your eye doctor will keep track of the pressure inside your eye.
Scatter laser surgery
This procedure creates up to 2,000 microscopic burns to treat areas where your retina has come away from your macula. This may cause aberrant blood vessels to shrink. Two or more sessions might be necessary. Your side, colour, or night vision may be diminished after laser surgery, but your central vision may be preserved. It will work best to obtain it before those new vessels bleed.
Vitrectomy
You could require this operation if blood vessels leak into your retina and vitreous humour and your eyesight becomes cloudy. It takes out the blood leak so you can see more clearly. This can clear up visual problems. You'll learn if any of these therapies are appropriate for you from your opthalmologist. They'll perform them in a hospital or a doctor's office.
Additional Read: World Diabetes Day
Complications For Diabetic Retinopathy
The development of aberrant blood vessels in the retina is a complication of diabetic retinopathy. Complications may result in severe eyesight issues:
Vitreous hemorrhage
The translucent, jelly-like fluid that fills the centre of your eye may leak from the new blood vessels. You could notice a few dark dots (floaters) if there is slight bleeding. However, blood can fill the vitreous cavity in more challenging situations, completely obstructing your vision. Usually, a vitreous haemorrhage does not result in permanent visual loss. Within a few weeks or months, the eye's blood usually stops being present. Your vision should regain its usual clarity, barring any retinal injury.
Retinal detachment
Scar tissue pulls the retina away from the back of the eye due to the aberrant blood vessels linked to diabetic retinopathy. This may result in floating dots in your field of vision, bright flashes, or severe vision loss.
Glaucoma
The iris, the portion of your eye in front, can develop new blood vessels that obstruct the fluid's natural passage out of the eye, increasing pressure inside the eye. The nerve that transmits images from your eye to your brain may be damaged by this pressure (optic nerve).
Blindness
Complete vision loss can result from diabetic retinopathy, macular oedema, glaucoma, or a combination of these disorders, mainly if the symptoms are poorly controlled.
Additional Read: Home Remedies To Control SugarDiabetes and high blood pressure or cholesterol increase your risk of developing diabetic retinopathy. Therefore, lowering your cholesterol and blood pressure can also help reduce your risk of losing your vision. Feel free to visit Bajaj Finserv Health if you need medical advice related to diabetic retinopathy from a professional. You can get an online doctor's consultation without having to visit and enjoy a healthy life ahead physically. If you want to protect yourself from diabetes you can avail diabetes health insurance.
References
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.cdc.gov/visionhealth/pdf/factsheet.pdf
Disclaimer
Please note that this article is solely meant for informational purposes and Bajaj Finserv Health Limited (“BFHL”) does not shoulder any responsibility of the views/advice/information expressed/given by the writer/reviewer/originator. This article should not be considered as a substitute for any medical advice, diagnosis or treatment. Always consult with your trusted physician/qualified healthcare professional to evaluate your medical condition. The above article has been reviewed by a qualified doctor and BFHL is not responsible for any damages for any information or services provided by any third party.